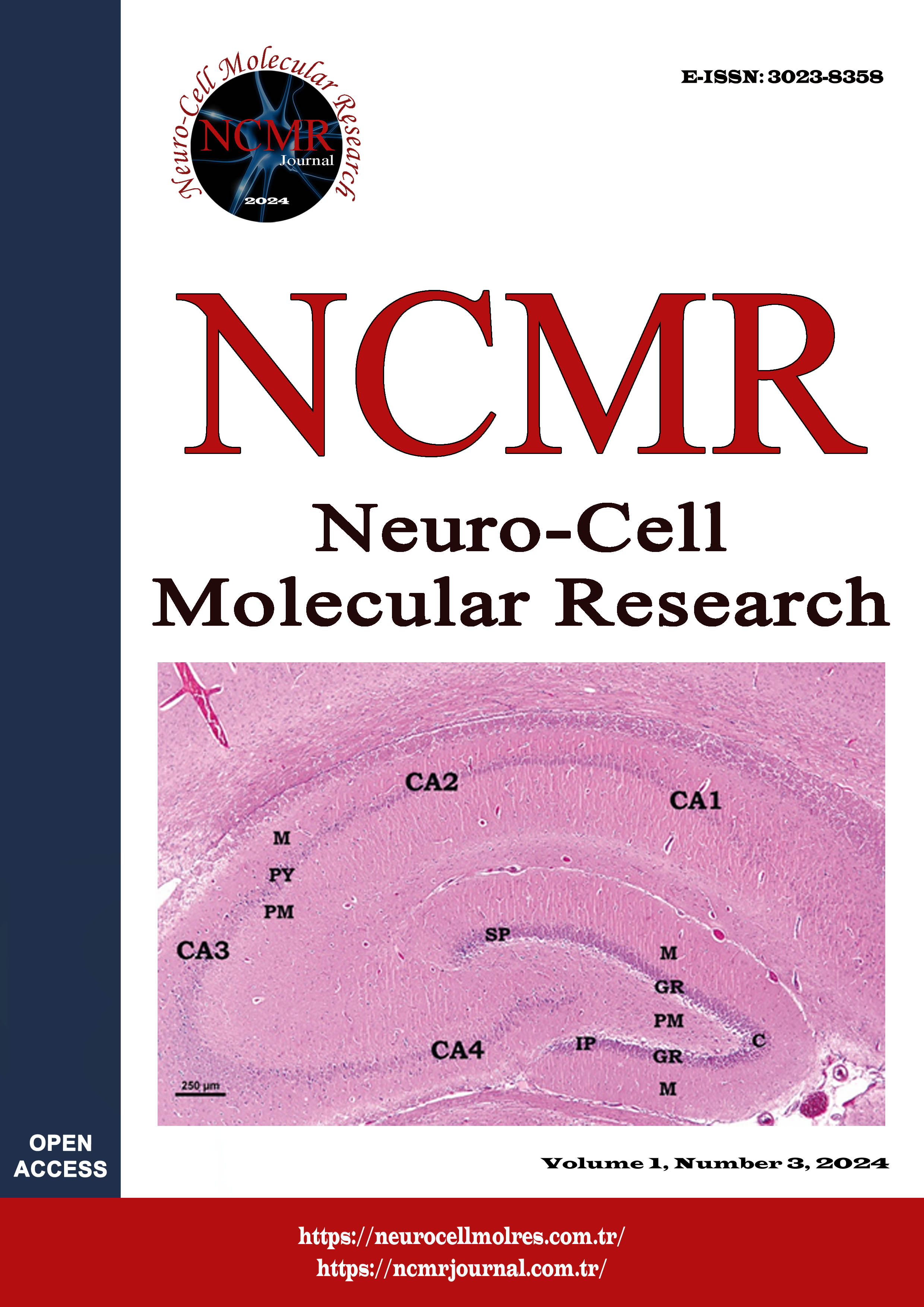
Protective effects of curcumin on the structure of the adrenal gland in diabetic rat model: A stereological, immunohistochemical and electron microscopic study
Protective Effects of Curcumin on the Diabetic Adrenal Gland
DOI:
https://doi.org/10.5281/zenodo.14552949Keywords:
Adrenal glands, curcumin, diabetes mellitus, rat, immunohistochemistryAbstract
This study investigated the ultrastructural changes in the adrenal gland in different stages of diabetes (onset, early, late) and the protective effects of curcumin. Seven groups of Wistar albino rats have six rats in each group. These were control, sham, curcumin, and four different Diabetes mellitus (DM) groups. For 14 days, the Sham group received corn oil, and the curcumin group received 30 mg/kg curcumin via intragastric gavage. DM group received a single dose of 50 mg/kg streptozotocin (STZ) I.P. for induction of diabetes. The DM-treated groups were given 30 mg/kg curcumin after seven days (DC1 group), after 21 days (DC2 group), and concurrently with STZ injection (DC3 group), respectively. Apoptotic processes in the adrenal gland were evaluated by immunohistochemistry.
Stereological analyses showed that the cortex volume of DM and DC2 groups was significantly increased compared to the Cont group. An increased medulla volume was also observed in the DM and DC2 groups. Histopathological analysis showed numerous lipid droplets and increased cytoplasmic density of cells in the zona fasciculata in the DM group. The adrenal gland showed a healthy structure in the early curcumin treatment group (DC1). Findings indicate that curcumin administration exhibits a protective effect on the structure of the diabetic adrenal gland. However, a late curcumin treatment did not provide a sufficient protective effect. Compared to other groups, a strong expression of anti-caspase-3 in the cortex and medulla of the adrenal gland belonging to the DM group was found. Our results showed that giving curcumin at the beginning of diabetes ameliorates the adrenal gland.
Downloads
References
Parsamanesh N, Moossavi M, Bahrami A, Butler AE, Sahebkar A. Therapeutic potential of curcumin in diabetic complications. Pharmacol Res. 2018; 136:181-193. https://doi.org/10.1016/j.phrs.2018.09.012.
Barber M, Kasturi BS, Austin ME, Patel KP, MohanKumar SM, MohanKumar PS. Diabetes-induced neuroendocrine changes in rats: role of brain monoamines, insulin and leptin. Brain Res. 2003; 964(1):128-35. https://doi.org/10.1016/s0006-8993(02)04091-x
Rudchenko A, Akude E, Cooper E. Synapses on sympathetic neurons and parasympathetic neurons differ in their vulnerability to diabetes. J Neurosci. 2014;34(26):8865-74.
https://doi.org/10.1523/JNEUROSCI.0033-14.2014
Chan O, Inouye K, Akirav EM, Park E, Riddell MC, Matthews SG, et al. Hyperglycemia does not increase basal hypothalamo-pituitary-adrenal activity in diabetes but it does impair the HPA response to insulin-induced hypoglycemia. Am J Physiol Regul Integr Comp Physiol. 2005;289 (1):R235-46. https://doi.org/10.1152/ajpregu.00674.2004
Stephens MA, Wand G. Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol Res. 2012;34(4):468-83. PMID: 23584113; PMCID: PMC3860380
Godoy-Matos AF, Vieira AR, Moreira RO, Coutinho WF, Carraro LM, Moreira DM, et al. The potential role of increased adrenal volume in the pathophysiology of obesity-related type 2 diabetes. J Endocrinol Invest. 2006;29(2): 159-63. https://doi.org/10.1007/BF03344090
Carsin-Vu A, Oubaya N, Mulé S, Janvier A, Delemer B, Soyer P, Hoeffel C. MDCT Linear and volumetric analysis of adrenal glands: Normative data and multiparametric assessment. Eur Radiol. 2016;26(8):2494-501. https://doi.org/10.1007/s00330-015-4063-y
Yang H, Du Z, Wang W, Song M, Sanidad K, Sukamtoh E, et al. Structure-activity relationship of curcumin: Role of the methoxy group in anti-inflammatory and anticolitis effects of curcumin. J Agric Food Chem. 2017;65(22):4509-4515. https://doi.org/10.1021/acs.jafc.7b01792
Avila-Rojas SH, Lira-León A, Aparicio-Trejo OE, Reyes-Fermín LM, Pedraza-Chaverri J. Role of autophagy on heavy metal-induced renal damage and the protective effects of curcumin in autophagy and kidney preservation. Medicina (Kaunas). 2019;10;55(7):360. https://doi.org/10.3390/medicina55070360
Lao CD, Ruffin MT 4th, Normolle D, Heath DD, Murray SI, Bailey JM, et al. Dose escalation of a curcuminoid formulation. BMC Complement Altern Med. 2006; 6:10. https://doi.org/10.1186/1472-6882-6-10.
Nabavi SF, Thiagarajan R, Rastrelli L, Daglia M, Sobarzo-Sánchez E, Alinezhad H, et al. Curcumin: a natural product for diabetes and its complications. Curr Top Med Chem. 2015;15(23):2445-55. https://doi.org/10.2174/1568026615666150619142519
Kandemir FM, Ozkaraca M, Küçükler S, Cağlayan C, Hanedan B. Preventive effects of hesperidin on diabetic nephropathy induced by streptozotocin via modulating TGF-β1 and oxidative DNA damage. Toxin Rev. 2017;(37):287–293.
https://doi.org/10.1080/15569543.2017.1364268
Breidert M, Böttner A, Möller S, Herberg L, Bornstein S. Apoptosis in the adrenal gland of non-obese diabetic (NOD) mice. Exp Clin Endocrinol Diabetes. 1998;106(6):478-83. https://doi.org/10.1055/s-0029-1212020.
Sharma S, Kulkarni SK, Agrewala JN, Chopra K. Curcumin attenuates thermal hyperalgesia in a diabetic mouse model of neuropathic pain. Eur J Pharmacol. 2006;536(3):256-61.
https://doi.org/10.1016/j.ejphar.2006.03.006
Tufekci KK, Kaplan S. Beneficial effects of curcumin in the diabetic rat ovary: a stereological and biochemical study. Histochem Cell Biol. 2023;159(5):401-430. https://doi.org/10.1007/s00418-022-02171-4
Zengin H, Kaplan S, Tümkaya L, Altunkaynak BZ, Rağbetli MÇ, Altunkaynak ME, Yilmaz O. Effect of prenatal exposure to diclofenac sodium on the male rat arteries: a stereological and histopathological study. Drug Chem Toxicol. 2013;36(1):67-78. https://doi.org/10.3109/01480545.2011.649287
Zaki SM, Abdelgawad FA, El-Shaarawy EAA, Radwan RAK, Aboul-Hoda BE. Stress-induced changes in the aged-rat adrenal cortex. Histological and histomorphometric study. Folia Morphol (Warsz). 2018; 77(4): 629-641. https://doi.org/10.5603/FM.a2018.0035
Baimai S, Bhanichkul P, Lanlua P, Niyomchan A, Sricharoenvej S. Modifications of adrenal gland ultrastructure in streptozotocin-induced diabetic model rats. Int J Morphol. 2021;39:109-115. https://doi.org/10.4067/S0717-95022021000100109
Badawy GM. Curcumin ameliorates the hazard effect of prenatal betamethasone administration on the fetal adrenal gland of albino rats. EJPMR. 2018;5(12): 133-148
Itoh N, Hanafusa T, Katsura H, Yamamoto K, Takeda A, Kurahashi A, et al. Two types of autoantibodies to adrenal medullary cells in type 1 (insulin-dependent) diabetic patients: prevalence, properties and implications. J Autoimmun. 1991;4(5):807-18.
https://doi.org/10.1016/0896-8411(91)90175-c
Wilke RA, Hillard CJ. Decreased adrenal medullary catecholamine release in spontaneously diabetic BB-Wistar rats. Role of hypoglycemia. Diabetes. 1994;43(5):724-9. https://doi.org/10.2337/diab.43.5.724.
Tülüce Y, Osmanoğlu D, Rağbetli MÇ, Altındağ F. Protective action of curcumin and alpha-lipoic acid, against experimental ultraviolet-A/B induced dermal-injury in rats. Cell Biochem Biophys. 2024; 82(4): 3535-46. https://doi.org/10.1007/s12013-024-01442-2
Rebuffat P, Belloni AS, Malendowicz LK, Mazzocchi G, Meneghelli V, Nussdorfer GG. Effects of streptozotocin-induced experimental diabetes on the morphology and function of the zona fasciculata of rat adrenal cortex. Virchows Arch B Cell Pathol Incl Mol Pathol. 1988;56(1):13-9. https://doi.org/10.1007/BF02889996
Noguchi S, Ohno Y, Aoki N. Adrenocortical insufficiency in Otsuka Long-Evans Tokushima Fatty rats, a type 2 diabetes mellitus model. Metabolism. 2007;56(10):1326-33.
https://doi.org/10.1016/j.metabol.2007.05.021
Elahi-Moghaddam Z, Behnam-Rassouli M, Mahdavi-Shahri N, Hajinejad-Boshroue R, Khajouee E. Comparative study on the effects of type 1 and type 2 diabetes on structural changes and hormonal output of the adrenal cortex in male Wistar rats. J Diabetes Metab Disord. 2013;12(1):9. https://doi.org/10.1186/2251-6581-12-9
Serifoglu I, Oz II, Bilici M. The adrenal gland volume measurements in manifestation of the metabolic status in type-2 diabetes mellitus patients. Int J Endocrinol. 2016;2016:7195849. https://doi.org/10.1155/2016/7195849
Chiodini I, Adda G, Scillitani A, Coletti F, Morelli V, Di Lembo S, Epaminonda P, Masserini B, Beck-Peccoz P, Orsi E, Ambrosi B, Arosio M. Cortisol secretion in patients with type 2 diabetes: Relationship with chronic complications. Diabetes Care. 2007;30(1):83-8. https://doi.org/10.2337/dc06-1267
Inouye KE, Chan O, Yue JT, Matthews SG, Vranic M. Effects of diabetes and recurrent hypoglycemia on the regulation of the sympathoadrenal system and hypothalamo-pituitary-adrenal axis. Am J Physiol Endocrinol Metab. 2005;288(2):E422-9. https://doi.org/10.1152/ajpendo.00389.2004
Revsin Y, van Wijk D, Saravia FE, Oitzl MS, De Nicola AF, de Kloet ER. Adrenal hypersensitivity precedes chronic hypercorticism in streptozotocin-induced diabetes mice. Endocrinology. 2008; 149(7):3531-9. https://doi.org/10.1210/en.2007-1340
Kanczkowski W, Sue M, Bornstein SR. Adrenal gland microenvironment and its involvement in the regulation of stress-induced hormone secretion during sepsis. Front Endocrinol (Lausanne). 2016;7:156. https://doi.org/10.3389/fendo.2016.00156
Sricharoenvej S, Boonprasop S, Lanlua P, Piyawinijwong S, Niyomchan A. Morphological and microvascular changes of the adrenal glands in streptozotocin-induced long-term diabetic rats. Ital J Anat Embryol. 2009;114(1):1-10. PMID: 19845276
Catalano-Iniesta L, Iglesias-Osma MC, Sánchez-Robledo V, Carretero-Hernández M, Blanco EJ, Carretero J, et al. Variations in adrenal gland medulla and dopamine effects induced by the lack of Irs2. J Physiol Biochem. 2018;74(4):667-677. https://doi.org/10.1007/s13105-018-0655-8
Xu Y, Ku B, Cui L, Li X, Barish PA, Foster TC, et al. Curcumin reverses impaired hippocampal neurogenesis and increases serotonin receptor 1A mRNA and brain-derived neurotrophic factor expression in chronically stressed rats. Brain Res. 2007;1162:9-18. https://doi.org/10.1016/j.brainres.2007.05.071
Liu D, Wang Z, Gao Z, Xie K, Zhang Q, Jiang H, et al. Effects of curcumin on learning and memory deficits, BDNF, and ERK protein expression in rats exposed to chronic unpredictable stress. Behav Brain Res. 2014; 271: 116-21. https://doi.org/10.1016/j.bbr.2014.05.068
Bhatia N, Jaggi AS, Singh N, Anand P, Dhawan R. Adaptogenic potential of curcumin in experimental chronic stress and chronic unpredictable stress-induced memory deficits and alterations in functional homeostasis. J Nat Med. 2011;65(3-4): 532-43. https://doi.org/10.1007/s11418-011-0535-9
Xu Y, Ku B, Tie L, Yao H, Jiang W, Ma X, et al. Curcumin reverses the effects of chronic stress on behavior, the HPA axis, BDNF expression and phosphorylation of CREB. Brain Res. 2006;1122(1):56-64. https://doi.org/10.1016/j.brainres.2006.09.009
Wang X, Zhang W, Zhou S. Multifaceted physiological and therapeutical impact of curcumin on hormone-related endocrine dysfunctions: A comprehensive review. Phytother Res. 2024;38(7):3307-3336. https://doi.org/10.1002/ptr.8208
Wei Y, Li H, Li Y, Zeng Y, Quan T, Leng Y, et al. Advances of curcumin in nervous system diseases: the effect of regulating oxidative stress and clinical studies. Front Pharmacol. 2024;15:1496661. https://doi.org/10.3389/fphar.2024.1496661